Is Fasting Good for High Blood Pressure
High blood pressure (hypertension) affects nearly one in three adults worldwide and is one of the leading risk factors for heart disease, stroke, and kidney failure. In recent years, fasting has gained attention not just as a weight loss strategy, but also as a potential natural therapy for improving heart health. But is fasting good for high blood pressure, or could it make things worse?
The answer depends on how fasting is done, individual health status, and whether it’s guided by evidence-based practices. This article explores how fasting affects blood pressure, reviews scientific research, and provides safe, practical guidance for people with hypertension.
What effect does fasting have on blood pressure?
2. What Is High Blood Pressure?
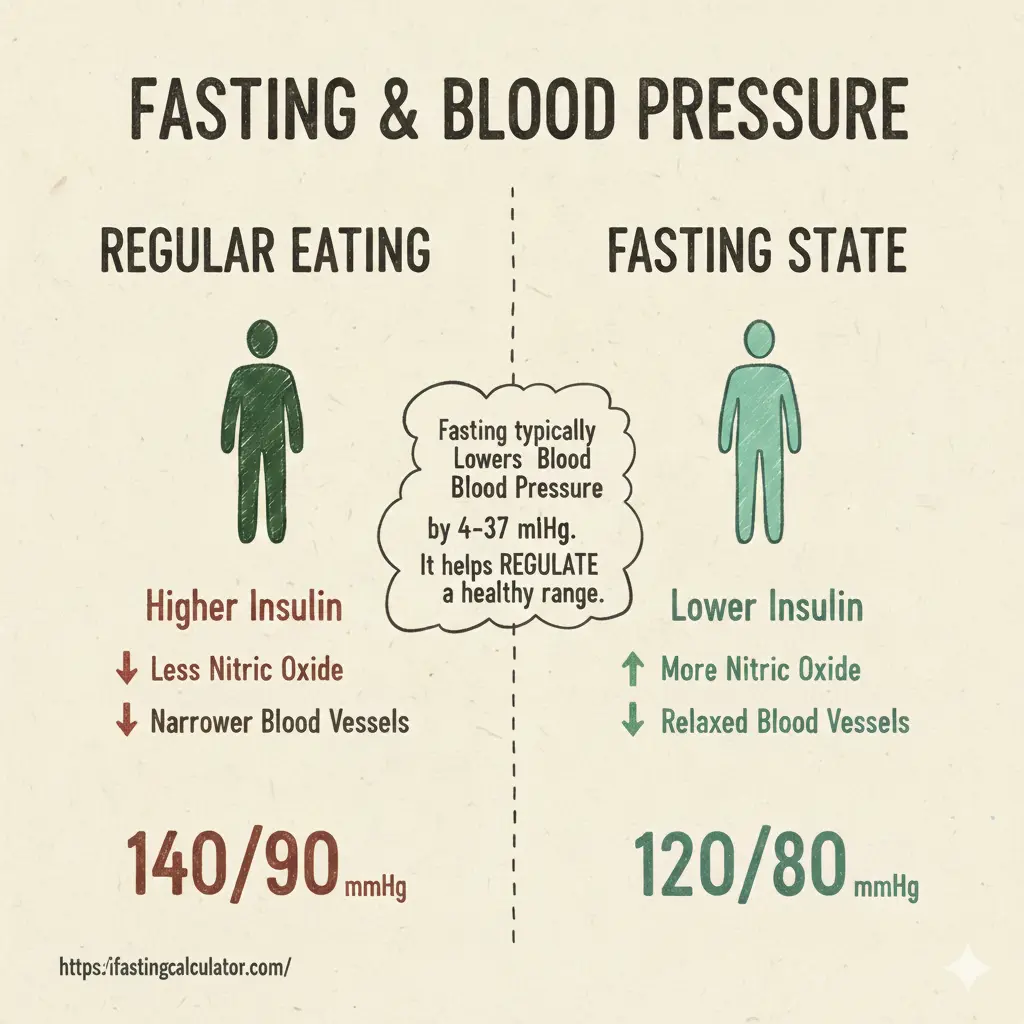
High blood pressure occurs when the force of blood pushing against your artery walls is consistently too high. Normal readings are around 120/80 mmHg. When the top number (systolic) exceeds 130, or the bottom (diastolic) goes over 80, you’re in the hypertensive range.
Persistent high blood pressure damages blood vessels, strains the heart, and contributes to chronic inflammation and organ stress. Lifestyle, diet, stress, and genetics all play roles — and that’s where fasting may intervene.
3. How Fasting Works in the Body
Fasting is more than just skipping meals. It triggers a series of metabolic changes that can influence blood pressure, cholesterol, and glucose control. When you fast:
- Insulin levels drop, improving fat metabolism.
- Blood sugar stabilizes, reducing vascular inflammation.
- Human growth hormone rises, supporting repair.
- Autophagy begins — the cellular “cleanup” process.
These changes can enhance cardiovascular efficiency and potentially help lower blood pressure, especially in people with insulin resistance or metabolic syndrome.
4. Types of Fasting (Intermittent, Water, Prolonged)
There are several fasting methods, each with unique effects:
- Intermittent Fasting (IF): Alternating periods of eating and fasting (e.g., 16:8 or 18:6 schedule).
- Water Fasting: Consuming only water for 24–72 hours.
- Prolonged Fasting: Going beyond 72 hours, often for therapeutic or religious reasons.
Among these, intermittent fasting has the most scientific support for safe, sustainable blood pressure improvements.
5. Can Fasting Lower Blood Pressure?
Multiple studies suggest that fasting can lower both systolic and diastolic pressure. A 2019 study in Nutrients found that participants practicing intermittent fasting saw a significant reduction in systolic blood pressure by 7–11 mmHg after 8 weeks.
Another 2021 Frontiers in Nutrition paper showed that fasting improved endothelial function — the ability of blood vessels to relax — which is crucial for healthy pressure regulation.
6. Mechanisms: How Fasting Affects the Cardiovascular System
Fasting lowers blood pressure through several physiological mechanisms:
- Improved Insulin Sensitivity: Reduces hyperinsulinemia, which otherwise triggers sodium retention and vessel constriction.
- Reduced Inflammation: Fasting decreases C-reactive protein (CRP), a marker linked to vascular damage.
- Better Lipid Profile: LDL cholesterol drops while HDL increases.
- Enhanced Nitric Oxide Production: Helps blood vessels dilate more efficiently.
- Lower Body Weight: Reduces strain on the heart and arteries.
7. Fasting and Insulin Sensitivity
High insulin levels drive both obesity and hypertension. Fasting reduces insulin resistance, allowing the body to use energy more efficiently. Improved insulin sensitivity leads to better sodium balance, reduced arterial stiffness, and more stable blood pressure.
8. Role of Weight Loss in Blood Pressure Control
Weight loss alone can lower systolic pressure by 1 mmHg for every 2 pounds lost. Since fasting promotes caloric restriction naturally, it helps achieve sustainable weight reduction. When combined with exercise and proper hydration, the effect on blood pressure is even stronger.
9. Fasting vs. Traditional Diets for Hypertension
Traditional low-sodium diets like the DASH (Dietary Approaches to Stop Hypertension) plan work well for many patients. However, fasting addresses hormonal imbalances and metabolic causes of hypertension that standard diets may overlook. The key advantage of fasting is that it doesn’t just reduce calories — it resets metabolic timing.
10. Water Fasting and Blood Pressure
Short-term water fasting under medical supervision has shown striking results. A study from the TrueNorth Health Center demonstrated that a 10-day water fast reduced average systolic pressure from 151 to 122 mmHg in hypertensive participants.
However, unsupervised water fasting can cause electrolyte imbalances and dehydration, both of which may increase blood pressure temporarily.
11. Intermittent Fasting for Hypertension: Research Insights
Intermittent fasting is generally safe and effective. People following 16:8 or 18:6 schedules often experience improvements in blood pressure, cholesterol, and resting heart rate. One mechanism may involve resetting the circadian rhythm, which influences blood pressure patterns throughout the day.
12. Fasting Risks for People with High Blood Pressure
Fasting isn’t suitable for everyone. Risks include:
- Dizziness or lightheadedness from low sodium or dehydration.
- Blood pressure spikes due to stress or missed medications.
- Nutrient deficiencies if fasting is prolonged without planning.
- Electrolyte disturbances leading to arrhythmias.
13. Managing Medication During Fasting
People taking antihypertensive medications should consult their physician before fasting. Some drugs (like diuretics) can amplify dehydration risk. Adjustments may be needed for safe fasting — for example, taking medication with small sips of water during fasting windows.
14. Who Should Avoid Fasting?
Fasting is not recommended for:
- People with severe hypertension (>180/110 mmHg)
- Those on multiple heart medications
- Pregnant or breastfeeding women
- Individuals with diabetes using insulin
- People with eating disorders or low BMI
15. Best Fasting Practices for Heart Health
If you’re considering fasting for blood pressure control:
- Start gradually with a 12:12 or 14:10 fasting schedule.
- Stay hydrated with water and electrolytes.
- Avoid processed foods during eating windows.
- Add potassium-rich foods (bananas, avocados).
- Exercise moderately — walking, yoga, or resistance training.
16. Lifestyle Changes That Support Blood Pressure Management
Fasting alone isn’t enough. Combine it with:
- Low-sodium diet (<2,300 mg/day)
- Regular physical activity
- Adequate sleep
- Stress management (meditation, breathing)
- Avoiding alcohol and smoking
17. Expert Opinions: What Cardiologists Say
Cardiologists acknowledge fasting as a promising adjunct therapy. Dr. Jason Fung and others have reported significant blood pressure improvements among patients combining intermittent fasting with balanced nutrition. Still, experts emphasize medical guidance and individualized plans.
How to Start Fasting Safely
- Get medical clearance.
- Choose a fasting schedule (start with 12 hours).
- Track blood pressure daily.
- Break the fast with whole, unprocessed foods.
- Stop fasting immediately if you feel unwell.
Final Thoughts: Is Fasting Good for High Blood Pressure?
The evidence suggests that fasting can help lower high blood pressure when practiced safely. It improves insulin sensitivity, reduces inflammation, and supports healthy weight — all essential for cardiovascular well-being. However, fasting is not a substitute for medication or medical advice. When done correctly, under supervision, it can be a powerful natural aid in maintaining healthy blood pressure.